The relationship between aging and cancer is complex and multifaceted. Aging is a significant risk factor for developing cancer, and this connection can be explained by several biological mechanisms:
-
Accumulation of Genetic Damage: As people age, their cells accumulate genetic mutations due to various factors such as environmental exposures (e.g., UV radiation, carcinogens) and cellular processes (e.g., DNA replication errors, oxidative stress). Over time, this genetic damage can disrupt normal cell functions, potentially leading to cancer.
-
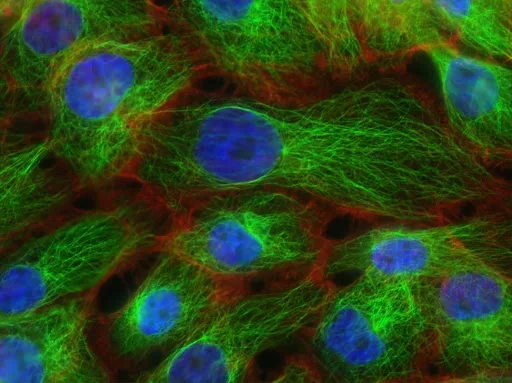
Cellular Senescence: Aging is associated with an increase in cellular senescence, a state in which cells lose their ability to divide. Senescent cells can accumulate in tissues and secrete pro-inflammatory molecules, creating a microenvironment that may promote cancer development and progression.
-
Weakened Immune System: The immune system becomes less efficient with age (a phenomenon known as immunosenescence), reducing its ability to detect and destroy cancerous cells. This diminished immune surveillance increases the risk of cancer.
-
Telomere Shortening: Telomeres are protective caps at the ends of chromosomes, which shorten with each cell division. Over time, telomere shortening can lead to chromosomal instability, a hallmark of cancer. Shortened telomeres may also lead to the activation of oncogenes or the loss of tumor suppressor gene function.
-
Changes in Tissue Microenvironment: Aging alters the tissue environment, including the extracellular matrix and blood vessels. These changes can create conditions that favor tumor growth and metastasis. For instance, aging can promote the chronic inflammation that is often seen in the tumor microenvironment.
-
Decreased DNA Repair Capacity: The ability of cells to repair DNA damage declines with age, making it more likely that mutations will persist, some of which may lead to cancer. This reduction in DNA repair is one of the reasons why older individuals are more prone to cancer.
Overall, while aging itself doesn't cause cancer, it creates conditions that increase the likelihood of genetic mutations and cellular abnormalities that can drive cancer development. This is why cancer incidence rises significantly with age.
Aging and cancer are distinct yet interconnected processes, each with unique characteristics and biological implications. Here’s a breakdown of their differences:
| Aspect | Aging | Cancer |
|---|---|---|
| Definition | The natural, progressive decline in physiological functions over time. | A disease characterized by uncontrolled cell growth and division, leading to tumor formation. |
| Nature | A normal, inevitable biological process. | A pathological condition caused by genetic and cellular abnormalities. |
| Cellular Behavior | Cells exhibit reduced division (senescence) and functional decline. | Cancer cells evade senescence and exhibit uncontrolled proliferation. |
| Genetic Changes | Accumulation of mutations is gradual, often without immediate consequences. | Mutations trigger oncogene activation or tumor suppressor gene inactivation, driving cancer. |
| Immune System Role | Immune function declines with age (immunosenescence), contributing to overall vulnerability. | Immune evasion by cancer cells allows their unchecked growth. |
| Telomere Dynamics | Telomeres shorten with each division, leading to aging and senescence. | Cancer cells often activate telomerase to maintain telomere length, supporting immortality. |
| Inflammation | Chronic, low-grade inflammation (inflammaging) is common. | Cancer thrives in an inflammatory environment, which supports tumor progression. |
| Impact on Body | Leads to functional decline across all systems (e.g., muscles, brain, heart). | Localized or systemic effects depending on cancer type, including tissue destruction. |
| Reversibility | Aging is irreversible (though its effects can sometimes be slowed). | Cancer can potentially be treated, managed, or cured in some cases. |
| Risk Factors | Intrinsic (genetics) and extrinsic (lifestyle, environment). | Mutations, carcinogens, infections, and genetic predispositions. |
Key Interconnection
- Aging increases the risk of cancer as accumulated mutations, a weakened immune system, and an altered microenvironment provide favorable conditions for cancer development. However, not all aging individuals develop cancer, highlighting the complex interplay of risk factors.