HIV and AIDS
Key Facts
HIV remains a significant global public health issue, having claimed an estimated 42.3 million lives to date, with ongoing transmission in all countries worldwide. As of the end of 2023, approximately 39.9 million people were living with HIV, with 65% residing in the WHO African Region.
In 2023, around 630,000 people died from HIV-related causes, and an estimated 1.3 million individuals acquired HIV. While there is currently no cure for HIV infection, effective prevention, diagnosis, treatment, and care—including for opportunistic infections—have made it manageable as a chronic health condition. This enables individuals living with HIV to lead long and healthy lives.
Organizations such as the WHO, the Global Fund, and UNAIDS have aligned their global HIV strategies with the Sustainable Development Goal (SDG) target 3.3, aimed at ending the HIV epidemic by 2030. By 2025, the goal is for 95% of all people living with HIV to be diagnosed, 95% of those diagnosed to receive lifesaving antiretroviral treatment, and 95% of those on treatment to achieve a suppressed viral load, which benefits their health and reduces HIV transmission. In 2023, the percentages for these targets were 86%, 89%, and 93%, respectively.
Of all people living with HIV in 2023, 86% were aware of their status, 77% were receiving antiretroviral therapy, and 72% had suppressed viral loads.
Overview
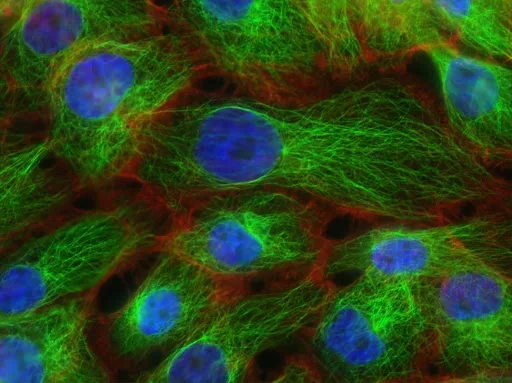
Human Immunodeficiency Virus (HIV) is a virus that attacks the body’s immune system. Acquired Immunodeficiency Syndrome (AIDS) represents the most advanced stage of HIV infection.
HIV specifically targets the body’s white blood cells, weakening the immune system and making it easier for individuals to become ill with diseases such as tuberculosis, infections, and certain types of cancer.
HIV is transmitted through the body fluids of an infected person, including blood, breast milk, semen, and vaginal fluids. It cannot be spread through casual contact such as kissing, hugging, or sharing food. HIV can also spread from a mother to her baby during childbirth or breastfeeding.
While untreated HIV can progress to AIDS over several years, it can be effectively prevented and treated with antiretroviral therapy (ART). The WHO defines Advanced HIV Disease (AHD) as having a CD4 cell count of fewer than 200 cells/mm³ or being classified as WHO stage 3 or 4 in adults and adolescents. All children younger than five years living with HIV are considered to have advanced HIV disease.
Signs and Symptoms
The symptoms of HIV vary depending on the stage of infection. The virus spreads more easily during the first few months after infection, although many individuals are unaware of their status until later stages. In the initial weeks post-infection, symptoms may be mild or resemble flu-like illness, including:
- Fever
- Headache
- Rash
- Sore throat
As the infection progresses, it increasingly weakens the immune system, leading to other signs and symptoms, such as:
- Swollen lymph nodes
- Weight loss
- Fever
- Diarrhea
- Cough
Without treatment, individuals living with HIV can develop severe illnesses, including:
- Tuberculosis (TB)
- Cryptococcal meningitis
- Severe bacterial infections
- Cancers, such as lymphomas and Kaposi's sarcoma
HIV can also exacerbate other infections, such as hepatitis C, hepatitis B, and mpox.
Transmission
HIV can be transmitted via the exchange of body fluids from individuals living with HIV, including blood, breast milk, semen, and vaginal secretions. It may also be transmitted to a child during pregnancy and delivery. Ordinary day-to-day contact such as kissing, hugging, shaking hands, or sharing personal items, food, or water does not transmit HIV.
People living with HIV who are taking ART and have an undetectable viral load cannot transmit HIV to their sexual partners. Early access to ART and support for adherence to treatment are critical not only for improving the health of those living with HIV but also for preventing HIV transmission.
Risk Factors
Certain behaviors and conditions increase the risk of contracting HIV, including:
- Engaging in anal or vaginal sex without a condom
- Having other sexually transmitted infections (STIs), such as syphilis, herpes, chlamydia, gonorrhea, and bacterial vaginosis
- The harmful use of alcohol or drugs in sexual contexts
- Sharing contaminated needles, syringes, and other injecting equipment
- Receiving unsafe injections, blood transfusions, or tissue transplants
- Undergoing medical procedures involving unsterile cutting or piercing, or experiencing accidental needle-stick injuries (including among healthcare workers)
Diagnosis
HIV can be diagnosed through rapid diagnostic tests that provide same-day results, facilitating early diagnosis and timely linkage to treatment and prevention services. Individuals can also use HIV self-tests for initial screening; however, confirmatory testing is required, which must be conducted by a qualified health worker or community worker.
- Most widely used HIV diagnostic tests detect antibodies produced by the body in response to HIV. These tests can detect HIV infection with high accuracy when using WHO prequalified tests within a nationally approved testing strategy and algorithm.
- having a voluntary medical male circumcision
- using harm reduction services for people who inject and use drugs.
Doctors may suggest medicines and medical devices to help prevent HIV infection, including:
- antiretroviral drugs (ARVs), including oral Pre-Exposure Prophylaxis (PrEP) and long acting products
- dapivirine vaginal rings
- injectable long acting cabotegravir.
ARVs can also be used to prevent mothers from passing HIV to their children.
People taking antiretroviral therapy (ART) and who have no evidence of virus in the blood will not pass HIV to their sexual partners. Access to testing and ART is an important part of preventing HIV.
Antiretroviral drugs given to people without HIV can prevent infection
When given before possible exposures to HIV it is called pre-exposure prophylaxis (PrEP) and when given after an exposure it is called post-exposure prophylaxis (PEP). People can use PrEP or PEP when the risk of contracting HIV is high; people should seek advice from a clinician when thinking about using PrEP or PEP.
Treatment
There is no cure for HIV infection. It is treated with antiretroviral drugs, which stop the virus from replicating in the body.
Current antiretroviral therapy (ART) does not cure HIV infection but allows a person’s immune system to get stronger. This helps them to fight other infections.
Currently, ART must be taken every day for the rest of a person’s life.
ART lowers the amount of the virus in a person’s body. This stops symptoms and allows people to live full and healthy lives. People living with HIV who are taking ART and who have no evidence of virus in the blood will not spread the virus to their sexual partners.
Pregnant women with HIV should have access to, and take, ART as soon as possible. This protects the health of the mother and will help prevent HIV transmission to the fetus before birth, or through breast milk.
Advanced HIV disease remains a persistent problem in the HIV response. WHO is supporting countries to implement the advanced HIV disease package of care to reduce illness and death. Newer HIV medicines and short course treatments for opportunistic infections like cryptococcal meningitis are being developed that may change the way people take ART and prevention medicines, including access to injectable formulations, in the future.
More information on HIV treatments
WHO response
Global health sector strategies on HIV, viral hepatitis, and sexually transmitted infections for the period 2022–2030 (GHSSs) guide strategic responses to achieve the goals of ending AIDS, viral hepatitis B and C, and sexually transmitted infections by 2030.
WHO’s Global HIV, Hepatitis and STIs Programmes recommend shared and disease-specific country actions supported by WHO and partners. They consider the epidemiological, technological, and contextual shifts of previous years, foster learning, and create opportunities to leverage innovation and new knowledge.
WHO’s programmes call to reach the people most affected and most at risk for each disease, and to address inequities. Under a framework of universal health coverage and primary health care, WHO’s programmes contribute to achieving the goals of the 2030 Agenda for Sustainable Development.